Prof. Dominique Caugant is part of a task force working towards defeating meningitis, alongside Meningitis Research Foundation. Here, she tells us about cutting edge sequencing technology that’s being used to trace a killer.
Norway experienced a long-lasting outbreak of meningococcal meningitis in the 1980s that triggered a lot of research at the Norwegian Institute of Public Health (NIPH) aiming to understand the epidemiology of this devastating disease and to develop vaccines in order to stop the epidemic. I started working at NIPH in that period and bacterial meningitis has been the focus of my research over more than 30 years.
Defeating meningitis is important to me because an otherwise healthy child with a great future in front of her/him may succumb to the disease in a few hours or, if surviving, may suffer from
sequelae for the rest of her/his life.
In spite of significant progress, especially with the development and increasing use of effective vaccines, much is required still to defeat meningitis on a worldwide basis.
What needs to happen?
To help defeat meningitis, we need to understand how these bacteria evolve and spread around the world so that the right vaccines can be used to prevent cases and the most at-risk population groups are vaccinated.
Neisseria meningitidis, which is responsible for large epidemics of meningococcal disease, is one of the most variable bacteria in nature. Most individuals will encounter the bacterium at one time or another in their life, but only a few people will develop disease. This is because the bacterium sometimes may acquire genes from close bacterial relatives, which helps them to adapt to different environments, and become more virulent and resistant to antibiotics.
This variability also makes it necessary to use different types of vaccines to protect people. Tracing the different strains and tracking the changes in their genetic material is essential so that appropriate vaccines can be deployed and we can understand how particularly virulent forms emerge and one day stop them in their tracks.
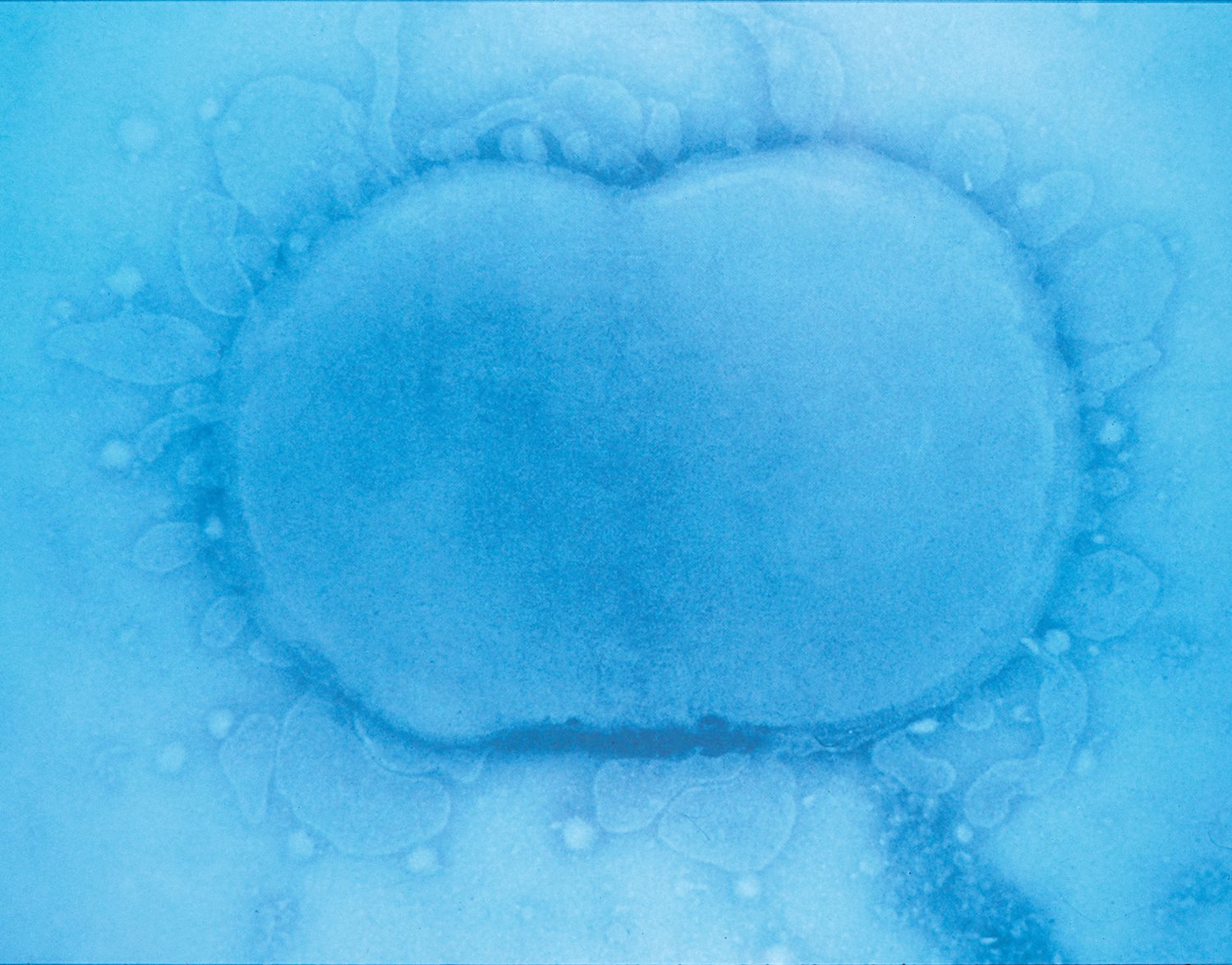 A meningococcal bacteria.
A meningococcal bacteria.
What milestones have you worked on?
Since 2010, over 300 million 1-29 year olds living in the African meningitis belt countries have been vaccinated against a type of meningitis bacteria, called MenA (meningococcal group A). We have been taking and analysing many thousands of samples from healthy people in Africa and have shown that the MenA strain basically has stopped circulating, but other types still do. It is thus vital to remain vigilant on emerging threats as meningitis is still occurring in this region and around the world.
We are using cutting edge sequencing technology to study the genetic makeup of meningitis causing bacteria, focusing on those collected from patients in the meningitis belt. For example, this allowed us to identify that small genetic changes, such as acquisition of a capsule (a ‘sugar-coat’ that can hide the bacteria from the human immune system) and a phage (a bundle of DNA that can confer potent disease-causing ability) by a non-virulent strain, can result in a new variant that may cause massive epidemics, as those that occurred in Niger and Nigeria in 2015 and again in 2017.
Next steps
To have a thorough understanding of the evolution and spread of meningitis causing pathogens, and to understand the full impact of different vaccines, large-scale collections of samples from different regions and dates need to be analysed by whole-genome sequencing and data interpreted using effective bioinformatics tools.
In recognition of the fact that meningitis is a global issue that urgently needs addressing, we are working with a group of international experts, expanding and connecting existing genome repositories, towards a Global Meningitis Genome Partnership that includes different meningitis causing pathogens. This intends to provide a resource with complete genetic blueprint of meningitis agents that can be accessed by researchers the world over.
These tools will be essential as we work with the World Health Organization and expert organisations to defeat meningitis by 2030.